Keratoconus
Understanding Keratoconus
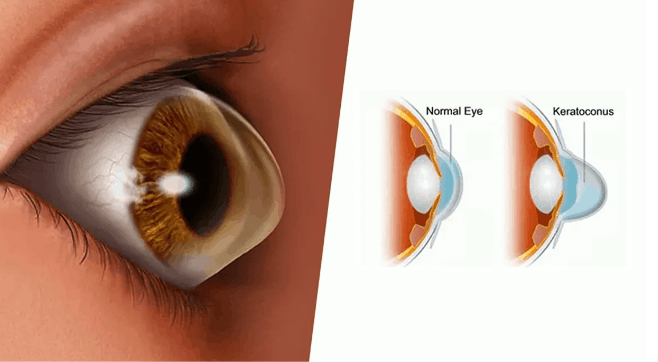
The cornea is the clear curved layer at the front of the eye. The precise shape of the cornea allows it to act as a lens, projecting an image into the eye. Sometimes the cornea is not strong enough to hold this round shape and it bulges outwards like a cone. This condition is called Keratoconus and it results in significant vision impairment. Symptoms usually start to occur in people who are in their late teens and early 20s. The treatment plan for Keratoconus has two aspects, first to stop its progression and second is to look at the refractive error and provide aid to improve the impaired vision. Severe cases may require corneal transplant. The word Keratoconus is formed by two Greek words: kerato, meaning cornea, and konus, meaning cone. Keratoconus is a condition in which the shape of the cornea, which is usually round, is distorted, developing a cone-shaped bulge, resulting in decreased or distorted vision. The condition is mostly bilateral and asymmetric – meaning that it usually affects both eyes; however one eye may be more affected than the other. Keratoconus is an inherited condition that sometimes skips generations. Its onset is usually during puberty and is often related to allergies (hay fever, asthma and eczema). The cornea is a bit more elastic than normal and tends to alter in shape and thins out becoming cone shaped. Rubbing the eyes can aggravate the condition. The typical patient with undiagnosed Keratoconus complains of deteriorating vision and frequent change in glasses. They may often report multiple images or ghosting of images and often relate a history of frequent refractive correction changes without much improvement in visual acuity. Patients may also report irritating symptoms such as intolerance to light (glare), photophobia and a recurrent foreign body sensation. Our centres are equipped with the latest corneal topography systems (Pentacam, Orbscan) to help in early detection and monitoring of keratoconous.. We offer Keratoconus treatment – Corneal collagen cross linking.
Symptoms
Signs and symptoms of keratoconus may change as the disease progresses.
They include:
Blurred or distorted vision·
Increased sensitivity to bright light and glare, which can cause problems with night driving·
A need for frequent changes in eyeglass prescriptions·
Sudden worsening or clouding of vision
When to see a doctor
See your eye doctor (ophthalmologist or optometrist) if your eyesight is worsening rapidly, which might be caused by an irregular curvature of the eye (astigmatism). He or she may also look for signs of keratoconus during routine eye exams.
Symptoms of Keratoconus
- Blurring of vision
- Glare
- Difficulty in night vision
- Double vision
- Frequent change of glasses
- Better near vision without the need for reading glasses
Corneal Cross Linking & Treatment
Treatment:
Keratoconus and corneal ectasia (thinning) are conditions where the cornea bulges and becomes ‘cone’ shaped. This results in impaired vision even with glasses. In the early stages, RPG contact lenses can be used, but if the patient is contact lens intolerant or the disease is progressive, then C3R is the treatment of choice.
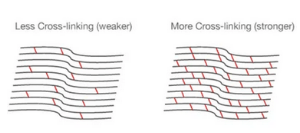
C3R is a new, non surgical, non invasive treatment. It works by strengthening the cornea by cross linking its building blocks (collagen). This can arrest the progression of keratoconus & has also been reported to partially reverse the corneal steepening that has already taken place.
What can I do to help my recovery?
The success of any surgical procedure depends on the recovery just as much as the procedure.
REST: The main thing you need to do is rest. Vision will be blurry for a while, so it’s difficult to read or watch TV. Most patients like to sleep or listen to music. Let the eye heal and don’t touch the contact lens.
AVOID INFECTION: In order to reduce the risk of infection, it is important to avoid contact with water for the first few days in particular (until your eye has healed). Your surgeon will be in the best position to advise you how long you should wait before swimming or performing heavy exercise. It is also essential to use your antibiotic drops as indicated. · MANAGE PAIN: Especially in the first day or two, stay on top of the pain. Use eye drops and take oral analgesics as advised by your surgeon.
C3R is a new, non surgical, non invasive treatment. It works by strengthening the cornea by cross linking its building blocks (collagen). This can arrest the progression of keratoconus & has also been reported to partially reverse the corneal steepening that has already taken place.
What can I expect after corneal cross linking?
It is really important that you understand that cross linking won’t make the vision clearer. In fact, it may be worse due to residual haze in the cornea for up to a year after treatment. Why have it then? You might ask. Good question. The fact is that corneal cross linking has been clearly shown to decrease the risk of corneal transplant. The younger you are when your keratoconus is diagnosed, the more rapidly your disease will progress and the sooner you will need a graft. Any treatment that avoids corneal transplant is good news. You’ve got to take the long term view here: vision may get temporarily worse, but it will improve slowly over the next year and – if you’ve had an effective treatment – the disease will have been halted or greatly slowed in its progression.
Frequently Asked Questions
The age of onset of keratoconus can vary from early teens to people in their 40’s or older. Although cases in which keratoconus is first diagnosed at an earlier age usually result in more advanced progression, it is not unusual for the disease to progress upto a certain point and then stablize. The continued thinning of the cornea usually progresses slowly for 5 to 10 years and then tends to stop. Occasionally, it is rapidly progressive.
Yes, in approximately 90% of keratoconus cases the disease will manifest itself in both eyes. The rate of progression and the timing of the onset of the disease however is typically different for each eye.
In its earliest stages, keratoconus causes slight blurring and distortion of vision and increased sensitivity to glare and light. These symptoms usually first appear in the late teens and early twenties.. Keratoconus patients can also experience light sensitivity, disturbed night vision, headaches from eye strain and reading problems. They may require frequent chane of glasses.
Astigmatism is a common condition where the curvature of one or more of the optical surfaces of the eye (the cornea and lens surfaces) are more “round” in one direction than the other. In “regular” astigmatism the maximum and minimum powers are aligned at 90 degrees to each other while in “irregular” astigmatism they do not align. An egg is a good example of a surface with “regular astigmatism”. Keratoconus is a degenerative condition where the cornea thins in certain areas. This can lead to astigmatism – often regular at first but becoming increasingly irregular as the disease progresses.
The cause of keratoconus is still unknown despite our long experience with it. There has been no shortage of speculation or study and numerous theories have been proposed. One scientific view is that keratoconus is developmental (i.e., genetic) in origin. This suggests that it is the consequence of an abnormality of growth, essentially a congenital defect.
